A European Union project in Austria, Belgium and Slovenia aims to strengthen the capacities of Member States for accessing EU funding that could be used to support health system reforms.
Text: Dietmar Schobel
Demographic change, the shortage of skilled labour, digitalisation and the green transformation are just some of the major challenges of our time, not least for health systems. Structural reforms are needed to cope with these challenges over the long term, and these in turn need investment.
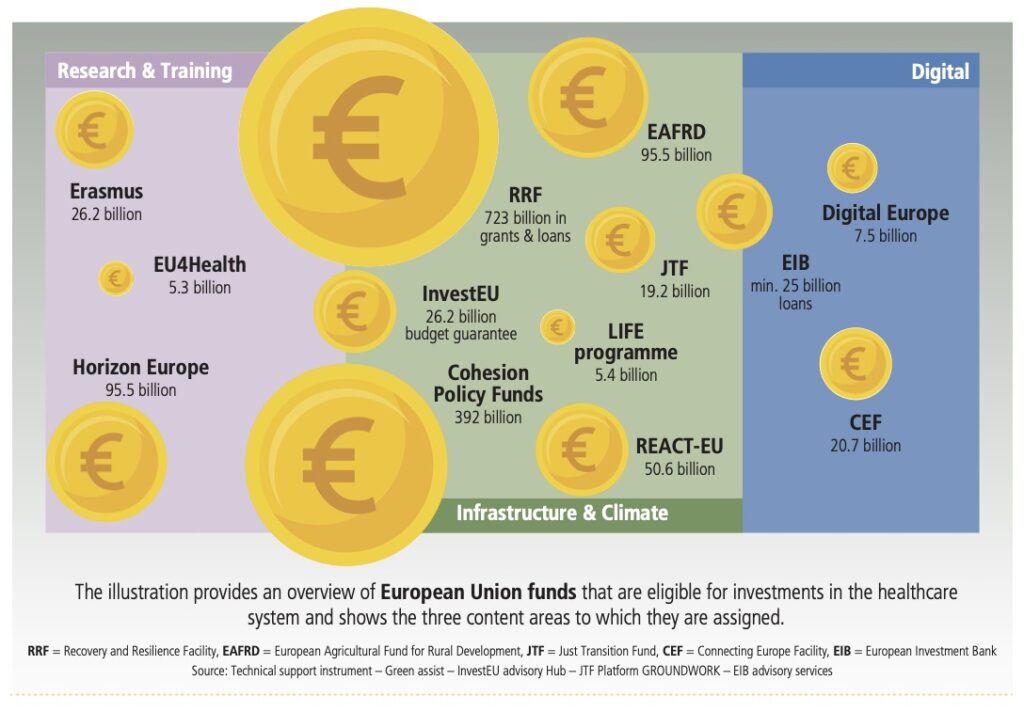
There is a broad range of funding instruments available at EU level that are eligible for this – from the €5.3 billion EU4Health programme to the €723 billion Recovery and Resilience Facility. These programmes target various objectives, from supporting research, training and digitalisation to promoting climate protection and improving infrastructure. In addition to financial support, some of them also provide technical assistance in the form of consulting services.
However, securing EU funding is not always the most straightforward process. Furthermore, individual EU funding programmes often do not prioritise health. This is why Austria, Belgium and Slovenia initiated the project Resources Hub for Sustainable Investing in Health within the European Union’s Technical Support Instrument (TSI) in 2022, to examine how existing EU funding instruments can be used more effectively for the health sector. This initiative is based on the Council Conclusions adopted during the Slovenian Presidency of the EU in 2021, which invited the Commission to enhance coordination of EU programmes and policies to better support national health system reforms and consider the provision of an advisory service for this purpose.
Two key pillars
“As many countries face similar challenges regarding their health systems, the health ministries in Austria, Belgium and Slovenia joined forces for this important TSI project, which is built on two main pillars,” explains Ilana Ventura, head of department for Healthcare Financing and International Affairs at the Austrian Ministry for Social Affairs, Health, Care and Consumer Protection.
These two key areas of focus were:
* Empowering the three Member States for making the case for public investment in health at national and EU level (see also box: “5 arguments for making the case for public investment in health”)
* Strengthening the capacity of the three Member States for accessing EU funding that could be used to support health system reforms by piloting a dedicated hub.
In the first pillar, the countries were supported in demonstrating the benefits of certain health investments or policies. For the second pillar, a pilot project was implemented in each of the three EU Member States, to test how existing EU funding instruments could be used for this purpose in practice. In this context, the European Observatory on Health Systems and Policies carried out mapping to identify relevant funding opportunities that matched the reform priorities of Austria, Belgium and Slovenia.
Three pilot projects
As the Austrian healthcare sector accounts for approximately 7 percent of the country’s CO2 emissions, the Austrian pilot project focusses on Greening Healthcare Facilities and supports a number of public hospital providers in Tyrol and Styria in identifying and applying to relevant EU funding instruments for their green investments.
In Belgium, a pilot project focussing on population health management has been implemented. Among other things, this has involved designing a digital dashboard for better integration of health and care data. This is one of the building blocks to support the implementation of a future inter-federal population health management strategy and better integrated care at loco-regional level.
The Slovenian pilot aims to strengthen primary healthcare in line with the strategy on primary care, which is in final stages of adoption. The goal is to improve access to primary care by expanding the scope of the existing national call centre to include telephone triage and advice. Setting up the national centre for development and coordination of primary healthcare is another objective. “In addition, we used the project to identify those parts of the proposed primary healthcare reform that could be eligible for EU funding and to create a roadmap for securing support during application procedures,” explains Dušan Jošar, head of unit, from the Health Ministry in Slovenia.
Benefits for all Member States
It is important to highlight that the TSI project is not just about creating more capacity in the three participating EU Member States. Rather, the intention is also to provide this kind of expertise for all Member States in the future by establishing an EU Health Hub: “This project has provided us with lots of valuable lessons learned and should ultimately serve as the basis for establishing an advisory hub at EU level that facilitates the use of EU resources by national authorities for sustainable investments in health,” concludes Anne Swaluë, International Relations Senior Expert from the Federal Ministry of Health in Belgium.
The project, implemented by Expertise France, the French public agency for international technical cooperation projects, will run until November 2024. A dedicated TSI flagship “EU Health Hub – Investing in Resilient Health Systems” has been launched for the TSI 2025 application cycle, and will build on the experiences of this project.
5 ARGUMENTS FOR MAKING THE CASE FOR PUBLIC INVESTMENT IN HEALTH
1. Health systems investments address health needs and improve health. Without adequate funding, there will be consequences for population health outcomes and well-being.
2. Health system investments further societal goals and have co-benefits beyond the health sector – for example, in the sectors of education, employment, economic, equity and social cohesion.
3. Health system financing can or will be sustainable following additional investment. Therefore, investments made now can serve to reduce costs later on.
4. The health system has the capacity to use additional resources effectively and efficiently.
5. The public (particularly voters), non-governmental organisations (NGOs), and civil society groups care about health and health system-related issues, and think more funding is needed.
Source: Rebecca Forman, Cameron Feil, and Jonathan Cylus: “A mapping exercise: making the case for public investment in health”. European Observatory on Health Systems and Policies, June 2023
